




Florida Blue Medicare Spotlight: 2025 Part D Changes and M3P Program
The Inflation Reduction Act (IRA) Brings Sweeping Changes for Florida Blue Customers in 2025.
Help your customers understand the changes for the coming year to best manage prescription costs.
Florida Blue Medicare Brokers should have all of the tools to help customers understand the benefits available to them for 2025. Below is a summary of changes as part of the Inflation Reduction Act, bringing flexible options to customers to manage their prescription costs.
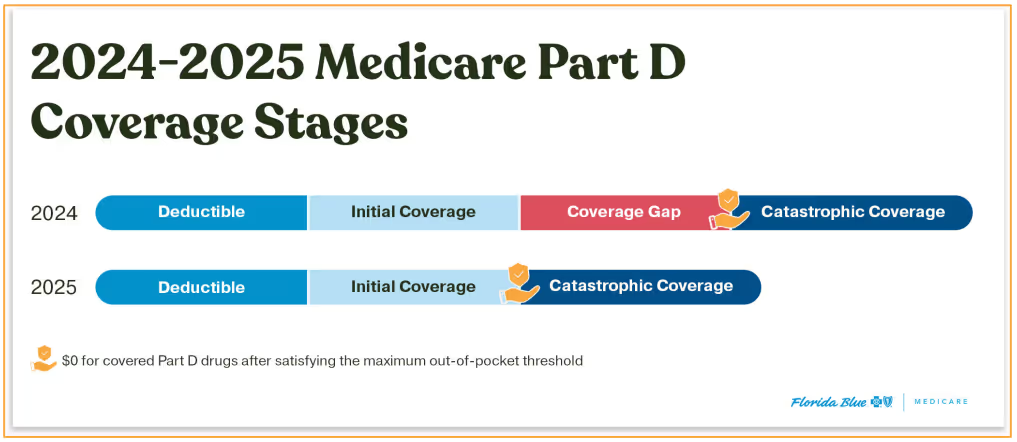
Out-of-pocket Expenses Capped at $2,000: Customers no longer experience a coverage gap between initial coverage and catastrophic coverage, with total OOP expenses limited to $2,000 for all beneficiaries starting in 2025.
Extra Help: Florida Blue offers Extra Help, a program that provides additional financial assistance to beneficiaries who qualify.
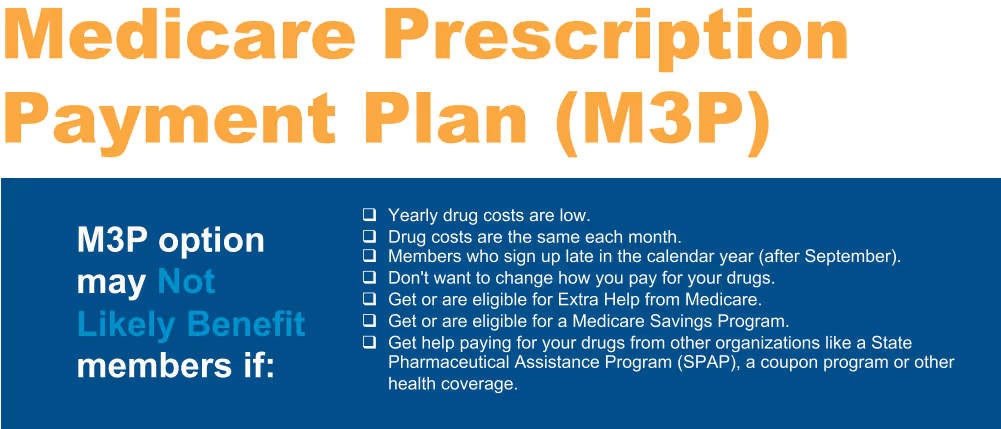
Availability of the Medicare Prescription Payment Plan (M3P): Separate from Extra Help, beneficiaries can enroll in the new Medicare Prescription Payment Plan (M3P) to help manage annual prescription drug costs. This is not a cost saving program, but rather a payment plan option for qualified beneficiaries to manage their costs annually.
What is the Medicare Prescription Payment Plan (M3P)?
Help members manage and pay prescription costs throughout the year
- The Medicare Prescription Payment Plan is a new payment option to help manage out-of-pocket Medicare Part D drug costs.
- The M3P program spreads drug costs across the calendar year (January-December).
- This payment option may help the member manage monthly expenses, but it doesn't save them money or lower drug costs.
- Starting in 2025, anyone with a Medicare drug plan or Medicare health plan with drug coverage (like a Medicare Advantage Plan with drug coverage) can use this payment option.
- Participation is voluntary.
- Members who opt-in would continue to pay plan premiums, if applicable.
- Instead of paying the pharmacy, opted-in members will get a bill from the health or drug plan to pay for their prescription drugs.
- Members are still responsible for their drug costs even though the member won't pay for drugs at the pharmacy
- There's no cost to participate in the Medicare Prescription Payment Plan.
Questions? Call us at 855-888-8326.
Don't have a MedicareValue page yet?
Get Your FREE Site >Posts you may be interested in...
 Read More
Read MoreMeet your California Broker Channel Manager: Sandy Wang
Meet your new Broker Channel Manager in California!
 Read More
Read MoreNew business technology is on the way for brokers!
These changes include a new contracting system for all brokers/agents, and a new commissions experience for MA/PDP users.
 Read More
Read MoreHighmark Important Updates: Medigap, SSBCI, and Delaware D-SNP Information
Medigap, SSBCI, and Delaware D-SNP Information
 Read More
Read MoreExtend Your Molina Selling Season to December 31!
AEP is coming to a close, but the Integrated Care SEP* can still be used
 Read More
Read MoreUnitedHealthcare: JarvisWRAP for December 1
AEP support, UCard shipments and SSBCI verification
 Read More
Read MoreCigna Broker Insights: November 2025 - Edition 11.2
Broker Insights: The newsletter for all Medicare brokers - 11.2
-01.png)
Who we are & what we do.
Choosing an FMO to work with is not just about having access to top insurance products and commissions, it’s about finding a one-on-one agent service that is prepared to meet your needs.
Get to know us, and see how we can help you take your business to the next level.

.svg)








