


Excellus BCBS Broker News Vol. 20 No. 7
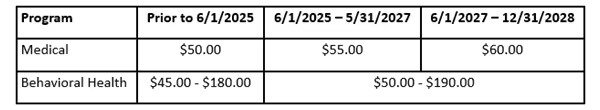
MDLIVE 6/1/2025 Increases
Excellus BlueCross BlueShield (BCBS) is excited to announce that they have renewed their partnership with their telemedicine partner, MDLIVE, for Medical and Behavioral Health telemedicine services through 12/31/2028.
As part of this multi-year renewal, the following fee schedule/allowable amount increases are effective 6/1/25. These increases are a direct result of the rising costs and demand for health care, which are having impacts both locally and nationally.
Member Out-of-Pocket Cost Share Impacts
- Non-HDHP Plans: There are no financial out-of-pocket cost share impacts to non-HDHP plans with copay or covered in full telemedicine benefits.
- HDHP Plans: Beginning August 1, members will be financially responsible for full out-of-pocket cost shares due at time of service for visits on or after August 1, 2025.
Common Questions:
- Does the cost increase impact group cost share?
- Yes, group cost share for MDLIVE will increase as a result of this change. While we are covering the balances that members would otherwise owe to MDLIVE, we are not covering the additional costs incurred at the group level.
- If a medical plan has a copay or covered in full telemedicine benefit, how does this increase impact enrolled members?
- Members enrolled in a medical plan with a copay or covered in full telemedicine benefit are not impacted by this increase. Impacted members would be those enrolled in a High Deductible Health Plan (HDHP) when their deductible or coinsurance has not been met yet at time of service.
- What happens if a HDHP member used MDLIVE services in the months of June or July 2025?
- If an HDHP member had a visit in June or July 2025, the cost share will remain the same as it was prior to June 1, 2025. They will not be responsible for the difference between the old and new pricing. Beginning August 1, 2025, HDHP members will need to pay the full new cost share for MDLIVE visits. Members will receive a letter soon so that they are aware of this change.
- Why is Excellus BCBS communicating this pricing increase after 6/1/25?
- Contract negotiations exceeded anticipated projected timelines ultimately impacting communications.
Any rate increase places a burden on members and employer partners. That’s why Excellus BlueCross BlueShield continues to partner with the broader health care system to identify opportunities to improve health outcomes and address rising costs. To learn more about our work on affordability, visit the new affordability page.
Large Group HMO And Medicare Supplement Rate Requests Filed With NYS
On July 1, 2025, an application was submitted requesting 2026 premium rate changes in accordance with New York state prior approval law. This rate application applies to Community Rated Large Group HMO. Additionally, an application was submitted requesting 2026 premium rate changes for Medicare Supplement products on June 13, 2025.
The following products are included in this 2026 rate filing:
- Blue Choice 25
- Blue Choice 30
- HMO Blue 25
- HMO Blue 30
- Medicare Supplement
Employer Group Communication
Initial notification letters will be mailed to community-rated employer groups and direct pay members enrolled in the products listed above. The letter will include the percentage change in premium rates that Excellus BlueCross BlueShield has requested in their application to New York state. The Department of Financial Services (DFS) will review the proposal and will determine the final approved rate levels which will be communicated later this year.
Broker Communication
Beginning in mid-July for Large Group HMO, you will receive an encrypted e-mail notification with copies of the initial notification letters being sent to your groups. The encrypted emails* will expire if not read within the specified timeframe as indicated in your email notification.
Your groups will receive an annual rate notification with the actual, approved rates 60 days prior to their renewal date. The annual rate notices will be available to Brokers on Information Connection.
It’s important that the groups receive the notification and distribute the individual letters to their employees with any additional information explaining the rate changes which may be different from the rates in the initial notification letters (e.g., shared expense).
Please contact your account consultant if you have any questions.
* Please Note: Encrypted files expire after a specified time from the send date. You will not be able to access the information in the file if the email isn't opened and read within that time. You will also be prompted to create a password associated with your email address to access the encrypted file.
Multi-factor Authentication Coming Soon For Broker And Employer Web Portals
Starting in early October, Excellus BlueCross BlueShield will be enabling multi-factor authentication for their broker portal. Multi-factor authentication is a way to ensure that the person attempting to log into to the web portal is truly them.
Implementing multi-factor authentication will not only prevent cyber threats and weaknesses for the company, but it will also protect your information and data within the web portal. It is also known as two-factor authentication, in which you need to confirm your identity via a one-time passcode.
What you can do to prepare for this change:
- Log into the broker portal and go to account settings
- Verify that your email address is up to date
- If needed, register a unique and current email address in the portal
- If several users each have their own login, but all use the same office email address, it is recommended to use email sub-addressing (e.g., office+john@example.com, office+mary@example.com) to create unique email addresses for each user. This helps ensure each account can be verified individually.
This will help alleviate login issues when the requirement is rolled out in the fall.
Multi-factor authentication will also be implemented for employer groups in September. Excellus BlueCross BlueShield will share this information in the July employer newsletter.
More detailed information will be released prior to the multi-factor authentication launch dates.
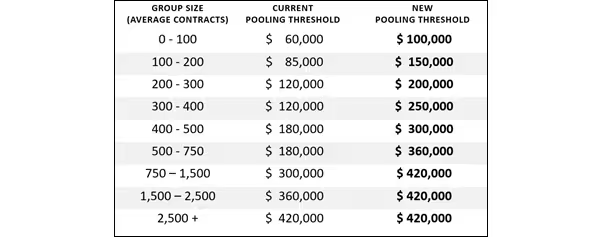
Experience-Rated Pooling Threshold Updates
Pooling thresholds for large group, experience-rated business are being revised. These updates will apply to quotes with effective dates on or after January 1, 2026. Please refer to the table below for the updated threshold amounts and their corresponding contract size ranges.
Pooling charges associated with the new thresholds will be applied on a per contract per month basis, consistent with current practice.
Pooling thresholds are regularly reviewed and periodically updated. Updating the thresholds provides a more accurate reflection of group experience and better aligns thresholds with today’s high-cost claimant environment.
If you have any questions, please contact your account service representative.
Pooling Threshold Table:
Using Incentives To Engage Employees In A Wellbeing Program
Incentives are a powerful tool for your clients’ wellbeing programs as they can motivate or encourage a desired behavior. Incentives can be anything from inexpensive raffle prizes to extra days off to reduced health care premiums or HSA contributions.
When used appropriately, they can motivate employees to adopt and maintain healthy behaviors that will improve their wellbeing. Adopting healthier behaviors is the key to minimizing health risks, lowering the prevalence of chronic disease, and improving overall wellbeing. Employees who feel better are more engaged in their work, contributing to improved productivity and lower turnover.
Incentives are the fastest way to increase participation in a wellbeing program, motivating even those employees who would not otherwise participate. A well-designed incentive strategy can be an important component of a comprehensive workplace wellbeing strategy, but the incentive should not be the whole program. An effective wellbeing strategy helps employees sustain healthy behaviors and includes understanding employees’ needs, engaging leadership, providing supportive resources, and creating a work environment that makes the healthy choice the easy choice.
The ultimate goal of an incentive program should be for employees to feel the benefits of their healthy behaviors and no longer need the external incentive. Although this won’t happen with every employee, incentives are a highly effective tool at nudging people down the path toward healthier behaviors.
To learn more about creating a best practice incentive strategy, refer to the resources provided or contact an Excellus BlueCross BlueShield account manager or wellbeing engagement consultant. The toolkit below includes an incentive best practice guide, communication templates, reporting criteria and metrics, healthy choices in the workplace guide and preventive services checklist.
Get the Best Practice Incentive Strategy Resource (ZIP)
Questions? Call us at 855-888-8326.
Don't have a MedicareValue page yet?
Get Your FREE Site >Posts you may be interested in...
 Read More
Read MoreMeet your California Broker Channel Manager: Sandy Wang
Meet your new Broker Channel Manager in California!
 Read More
Read MoreNew business technology is on the way for brokers!
These changes include a new contracting system for all brokers/agents, and a new commissions experience for MA/PDP users.
 Read More
Read MoreHighmark Important Updates: Medigap, SSBCI, and Delaware D-SNP Information
Medigap, SSBCI, and Delaware D-SNP Information
 Read More
Read MoreExtend Your Molina Selling Season to December 31!
AEP is coming to a close, but the Integrated Care SEP* can still be used
 Read More
Read MoreUnitedHealthcare: JarvisWRAP for December 1
AEP support, UCard shipments and SSBCI verification
 Read More
Read MoreCigna Broker Insights: November 2025 - Edition 11.2
Broker Insights: The newsletter for all Medicare brokers - 11.2
-01.png)
Who we are & what we do.
Choosing an FMO to work with is not just about having access to top insurance products and commissions, it’s about finding a one-on-one agent service that is prepared to meet your needs.
Get to know us, and see how we can help you take your business to the next level.

.svg)








